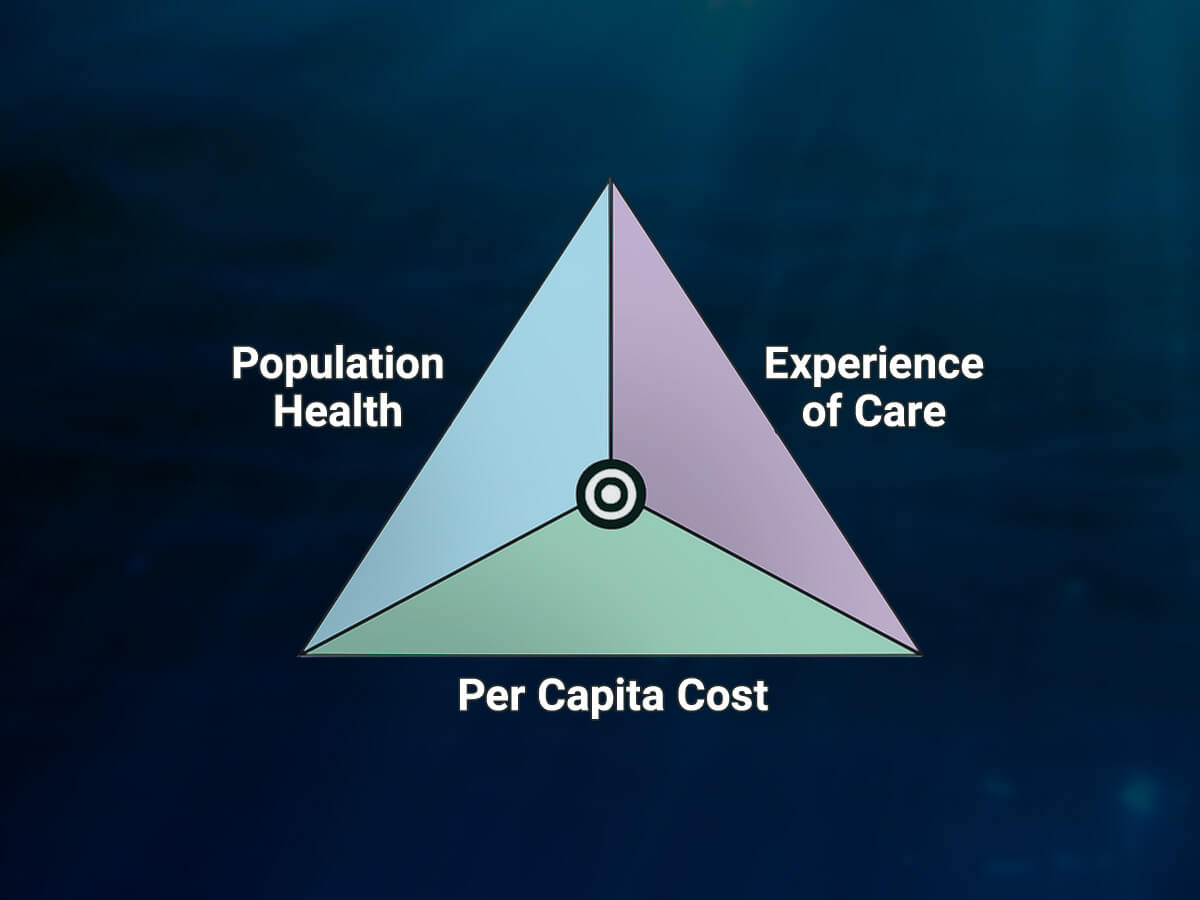
Since the passage of the Affordable Care Act in 2010, New York State has worked diligently to improve healthcare for all New Yorkers. To support this effort, decision makers and stakeholders have implemented policies in line with the Triple Aim to improve patient experience and population health while reducing healthcare costs.
One major change taking place in New York is the transition of Medicaid to managed care for behavioral health services from the previous fee-for-service system, which will improve care coordination, increase continuity of services, and emphasize preventative services.
On October 1, 2015, the NYC behavioral health system transitioned adult Medicaid clients to managed care, and the rest of the state will follow on July 1, 2016. In anticipation of this transition, the State-funded, McSilver Institute-directed Managed Care Technical Assistance Center (MCTAC) has worked to prepare the nearly 900 behavioral health agencies for these system-wide changes through webinars, in-person forums, learning communities, and tool development. The MCO Plan Comparison Matrix, interactive online glossary, and consultant directory, for example, have each helped providers navigate critical elements of the changing healthcare landscape. From MCTAC’s launch in September 2014 through February 2016, 300 OASAS agencies (70.9%) and 441 OMH agencies (79.9%) have participated in a training online or in-person or completed a managed care readiness assessment.
Similar to the adult system transition, MCTAC is now turning its focus to prepare child-serving providers throughout the state for significant changes. The transition to Medicaid managed care for children and teens under the age of 21 is scheduled to begin January 1, 2017, in New York City and Long Island and on July 1, 2017, for children in the rest of the state. Significantly, the implementation of Home and Community Based Services (HCBS) and State Plan Amendment (SPA) services will give an increased number of eligible children access to a wider scope of treatment opportunities.
In early 2016, a three-part webinar series, Transforming the Children’s Medicaid System, was held in partnership with New York State’s Department of Health (DOH), Office of Mental Health (OMH), Office of Alcoholism and Substance Use Services (OASAS), and Office of Children and Family Services (OCFS), to assist providers in understanding the changes that will be taking place and illustrating how providers can prepare for 2017. The three webinars attracted over 1,500 individuals over the course of the series, representing 229 unique behavioral health agencies. In addition, MCTAC has been hosting eight half-day forums throughout New York State during March and April. These in-person presentations expand on topics discussed in the webinar series and offer implementation guidance for the children’s transition.
As 2017 approaches, numerous web-based and in-person training opportunities will be offered similar to the technical assistance provided for adult behavioral health providers, focusing on key domains of managed care readiness including contracting, revenue cycle management, utilization management, outcomes, billing, and other topics. MCTAC partners will be working closely with the state, Managed Care Organizations, providers, and other stakeholders to adapt and tailor materials to have the greatest impact and relevance for child-serving agencies. MCTAC will also develop additional tools and resources to assist providers with the children’s system transformation.
For more information about upcoming trainings, tools, resources, and updates about New York State’s transition to Medicaid managed care, visit www.mctac.org and sign up for updates here.
This article contributed especially by Cassandra Stanton, Morgan McGuire, Caitlin Cronin, and Dan Ferris